Preventing HIV with Pharmacist-Prescribed PrEP
Author
Media Contact
For general and media inquiries and to book our experts, please contact: pr@rstreet.org
Introduction
In 2021, an estimated 32,100 Americans were infected with human immunodeficiency virus (HIV). The Department of Health and Human Services’ 2019 taskforce “Ending the HIV Epidemic in the United States” (EHE) aims to decrease new HIV infections to 9,300 cases by 2025 and 3,000 cases by 2030. Although the number of new HIV infections in the United States has been decreasing, significant progress is necessary to meet these targets.
Individuals can minimize their risk of acquiring HIV by using a number of harm reduction strategies. For people who inject drugs, using sterile injection equipment can prevent HIV transmission. Similarly, using condoms consistently and properly can prevent HIV transmission through sex. These strategies were among the main methods of reducing HIV transmission until 2012 when the U.S. Food and Drug Administration (FDA) first approved pre-exposure prophylaxis (PrEP) for the prevention of HIV among HIV-negative individuals. Currently, PrEP is available as a daily oral pill or a long-acting injectable. When used as directed, PrEP is extraordinarily effective at preventing HIV infection, reducing the risk of getting HIV from sex and injection drug use by about 99 percent and 74 percent, respectively.
Although PrEP use has increased dramatically among some demographic groups, there are significant differences in PrEP use by race, sex/gender, and sexual orientation. These differences are due to many factors, including HIV-related stigma; homophobia and transphobia; provider accessibility and hesitancy or unwillingness to prescribe; and individual perception of HIV risk. Although at-risk individuals should proactively take steps to decrease their risk of acquiring HIV, implementing the right polices can help overcome some of the barriers.
The EHE set a goal that 50 percent of people who could benefit from PrEP would have a prescription by 2025. Achieving this target will require multiple policy and social interventions. A key policy mechanism that could increase PrEP accessibility is expanding pharmacists’ scope of practice to include prescribing PrEP directly to a client, without involving another prescribing health care provider. Policies that facilitate pharmacist prescribing have the potential to help more people use PrEP, which can decrease health care costs by averting new HIV infections.
Preventing HIV with
Pharmacist-Prescribed PrEP
Policies that facilitate pharmacist prescribing have the potential to help more people use PrEP, which can decrease health care costs by preventing new HIV infections.
Pharmacy Access Models
Pharmacies are some of the most accessible points of health care delivery in the nation, with about 89 percent of Americans living within 5 miles of a pharmacy. Additionally, American consumers report that, if it meant lower health care costs, they would trust pharmacists to deliver health care services and prescribe medications. These factors make pharmacies and pharmacists an ideal addition to the PrEP-prescribing landscape.
Legal mechanisms that allow pharmacists to prescribe PrEP and other medications can be loosely grouped into two categories: delegated prescribing and independent prescribing. Delegated prescribing, often through a collaborative practice agreement (CPA), means that a health care provider with prescriptive authority (usually a physician) authorizes a pharmacist to perform certain elements of patient care (in this case, issue a prescription). Pharmacists can negotiate CPAs for an individual patient or a specific patient population, depending on the needs of the providers and patient(s), as well as state law. Because a pharmacist must find another provider to issue the CPA, this mechanism requires extra initiative from individual providers.
Independent prescribing, sometimes called direct prescribing, can be authorized through a statewide standing order or protocol or through legislation that provides a framework of criteria that dictate the circumstances in which a pharmacist can prescribe. The most important difference between the two mechanisms is that statewide standing orders or protocols usually apply to one medication or one class of medications, while the framework model is more general and can apply to a broader range of medications.
For the purposes of this analysis, we chose to focus on the 14 states that have authorized independent prescribing of PrEP through legislation codified by Dec. 31, 2023 (Table 1), although implementation of the legislation may not have occurred immediately. Laws governing CPAs are significantly more heterogeneous and often are not specific to PrEP, making it difficult to know if pharmacists in states that allow CPAs are using them to facilitate PrEP prescriptions. For these reasons, we did not include states that allow pharmacists to prescribe through CPAs in this analysis.
Table 1: States that have Authorized Independent Prescribing Of PrEP
| State | Year Legislation Passed |
|---|---|
| Arkansas | 2023 |
| California | 2019 |
| Colorado | 2020 |
| Connecticut | 2023 |
| Idaho | 2019 |
| Illinois | 2023 |
| Maine | 2021 |
| Montana | 2023 |
| Nevada | 2021 |
| New Mexico | 2023 |
| Oregon | 2021 |
| Rhode Island | 2023 |
| Utah | 2021 |
| Virginia | 2021 |
Western states have led the way in expanding pharmacists’ scope of practice related to PrEP, with states in the Midwest and along the East Coast adopting this legislation more slowly. The first states to enable independent prescribing of PrEP were Idaho and California in 2019. Most states that adopted this legislation did so in 2021 and 2023.
Of the states that have authorized independent prescribing of PrEP, most gave this authority through a statewide standing order or protocol. Montana and Idaho are exceptions, as they adopted the framework model, allowing pharmacists to prescribe any medication that meets a set of criteria laid out by the board of pharmacy. This means that Idaho and Montana’s legislation is not specifically related to PrEP, but pharmacists are allowed to prescribe PrEP because it meets the stated criteria. Illinois’ prescribing law is also different because it requires pharmacists to get a prescriber to issue a standing order for PrEP, rather than there being a statewide standing order or protocol. Because the standing order is an arrangement between a pharmacist and another medical provider, in some ways the law is more similar to laws that allow pharmacist prescribing through non-patient-specific CPAs. We included Illinois in the analysis because the law allows the Illinois Department of Public Health to issue a standing order, although they have not done so as of April 2024.
HIV and PrEP Statistics Analyzed
To assess geographic trends in HIV-and PrEP-related statistics, we used data from multiple sources. This section discusses state-level HIV and PrEP statistics compiled from our analysis to identify geographic trends in unmet need and pharmacist prescribing. We briefly describe key definitions for terms that will be used in this discussion in Table 2.
Table 2: Variables and Definitions
| Variable | Definition |
|---|---|
| Independent Prescriptive Authority | The ability for pharmacists to provide an initial PrEP prescription for a patient without collaborating with another medical provider who has prescriptive authority. Relates to how pharmacists’ scope of practice is defined. |
| PrEP-to-Need Ratio (PNR) | The ratio of the number of PrEP users in a given year to the number of people newly diagnosed with HIV in a given year. This metric assesses if PrEP use matches a populations needs for HIV prevention. A lower value means there is greater unmet need. |
| PrEP Coverage | The estimated percentage of people who could benefit from PrEP who have been prescribed PrEP. |
Since the ultimate goal of PrEP is to prevent people from acquiring HIV, it is informative to assess the HIV diagnosis rates in states that have allowed independent PrEP prescribing compared to those that have not. In general, HIV diagnosis rates are highest in the southern states. Among the states that allow independent PrEP prescribing, Nevada has the highest HIV diagnosis rate (18.9 per 100,000 people). Five of the 14 states that allow independent PrEP prescribing are among the states with comparatively low HIV rates (less than or equal to 5.5 per 100,000 people). Notably, the southern states, many of which have high diagnosis rates, are not expanding access through independent pharmacist prescribing.
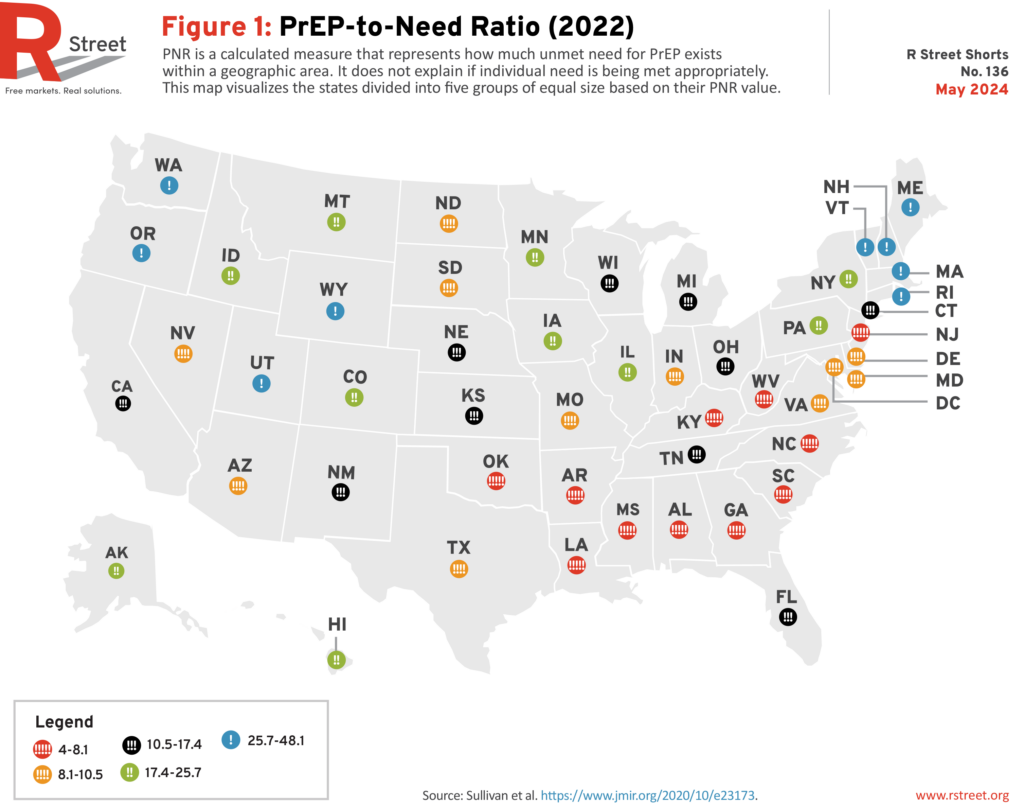
The PNR assesses PrEP use relative to new HIV diagnoses. Figure 1 shows each state’s 2022 PNR. Once again, the states with the greatest unmet need are concentrated in the South, but there are several Midwestern states also register a relatively high unmet need. Of the states that have passed independent PrEP prescribing legislation, four out of 14 are among the states where there is the lowest unmet need for PrEP, suggesting that those states recognized the potential benefits of expanding pharmacy-based PrEP access even with comparatively low unmet need.
Looking at the health care provider landscape is also informative when assessing the potential impact of independent PrEP prescribing. Primary care providers (PCPs) are the front line for getting PrEP prescriptions to the patients who can benefit from them. But no state has enough PCPs to meet their populations’ needs fully. Rhode Island has the highest percent of need met at 72.1 percent, but that still leaves a substantial gap to fill. Furthermore, not all PCPs prescribe PrEP; the reasons for this are varied, but there is evidence that 55 to 72 percent of PCPs are unwilling to prescribe the medication. In fact, in 2019, only 13.6 percent of general practice/family medicine physicians, 8.1 percent of internal medicine physicians, 4.5 percent of nurse practitioners, and 4.1 percent of physician assistants prescribed PrEP. Though these are increases from 2014, significant gaps remain.
Additionally, PrEP prescribers are not evenly distributed throughout the country, with most practicing in urban areas. The ratio of PrEP providers to people who could benefit from PrEP is lowest in the South, where there is a high unmet need for PrEP. For example, one study conducted in the South found that more than 50 percent of counties and zip code tabulated areas did not have an existing PrEP provider, whereas only 14 percent did not have a pharmacy. Given these statistics, there is a clear need to find ways to expand access to PrEP outside of primary care settings, such as through pharmacist prescribing.
We also conducted analyses to assess the individual associations between HIV diagnosis rate, PrEP coverage, PNR, and percent of PCP need met and a state having passed independent prescribing legislation. We did not find a statistical association between any of these variables and a state having passed independent prescribing legislation. It is important to note that many factors affect HIV diagnosis rates, PrEP coverage, and PNR, making it challenging to link any individual policy change to differences in these variables. Additionally, the lag in HIV data reporting, along with how recently many states had passed the relevant legislation, limited the possible analyses. Due to these limitations, we did not seek to evaluate the impact of codifying independent prescribing legislation based on any of these variables.
Why Policymakers Should Want to Expand PrEP Access
The United States has the tools to achieve the EHE goal of reducing HIV infections by 90 percent by 2030. Increasing PrEP use among people who could benefit from the medication is a key step toward meeting this goal. In fact, recent research found that as PrEP coverage in states increased, new HIV diagnoses decreased. Other studies have found that people who live in areas with more PrEP-prescribing locations are more willing to use PrEP. Preventing HIV infection improves community health, but it benefits society in other ways, too. Expanding access to PrEP can decrease medical costs by averting new HIV infections, increase consumer choice of PrEP access points, and decrease the strain on the primary care system.
Medical Costs
Helping people avoid getting HIV decreases the human cost of managing a chronic illness, and it decreases medical costs. One only has to look at the difference between government spending related to disease treatment and disease prevention to appreciate the need to give equal priority to both. In 2022, the federal government budgeted $28.7 billion for health care services and treatment for people living with HIV, yet only $1.1 billion went to HIV prevention. A 2022 report estimated that at the population level, the drug and ancillary costs (i.e, lab testing and clinic visits) of getting at least 50 percent of eligible people to use PrEP (the EHE goal) would be about $1.4 billion over 10 years. The report estimates that an additional $4.75 billion over 10 years would be required to conduct outreach and education to get to the 50 percent goal. However, just the medical savings associated the new HIV cases avoided by reaching the 50 percent target would amount to more than $2.27 billion over 10 years. Using this analysis, the medical savings for preventing HIV cases would more than cover the direct medical costs of increasing PrEP coverage to 50 percent.
Consumer Choice
Consumer surveys have confirmed that there is interest in and willingness to access PrEP services through pharmacies. In a small survey of 49 people currently receiving PrEP at a specialty pharmacy in Arizona, about 84 percent agreed that they would be comfortable having a pharmacist provide their initial PrEP prescription. Similarly, another survey of the general population found that 58.1 percent of respondents had no concerns with pharmacists prescribing PrEP. In both surveys, common reasons for being concerned about pharmacists independently prescribing PrEP included having a closer relationship with their physician, pharmacists’ level of training, and privacy considerations.
Although some individuals have concerns about pharmacist-prescribed PrEP, others also have concerns about securing PrEP from a PCP. In one survey, 80 percent of men who have sex with men said that they did not want to talk to their PCP about PrEP. 45 However, a different survey found that 80 percent of men who expressed concerns about accessing health care services because someone might find out that they have sex with men were willing to be screened for PrEP at a pharmacy.46 With this juxtaposition in mind, allowing pharmacist-prescribed PrEP would give patients the ability to choose between familiarity (PCP prescribed) and anonymity (pharmacist prescribed) depending on the needs of the patient. Finally, despite some people expressing discomfort with pharmacist prescribing, all of the respondents in the Arizona survey felt that allowing pharmacists to prescribe PrEP would benefit their community.
Health Care Workforce Considerations
The Association of American Medical Colleges predicts that by 2034, the United States will be short between 17,800 and 48,000 PCPs. For this reason, finding ways to better utilize all medical providers, including pharmacists, is vital. A 2023 study quantified how expanding PrEP access through pharmacies could expand access to the medication in southern states. The study found that PrEP prescribing locations in the South could increase 80.9 fold by integrating pharmacies into the HIV prevention care landscape.
Equally important as workforce statistics are pharmacists’ attitudes toward prescribing PrEP. A survey of California pharmacists found that 96 percent said pharmacy-based PrEP and post-exposure prophylaxis (PEP) was important, and 81 percent were willing to prescribe these medications to clients. Another survey of pharmacists in South Carolina found that 86 percent would be willing to prescribe PrEP.
Another important consideration about expanding pharmacists’ independent prescribing authority is whether pharmacists are knowledgeable enough about PrEP to prescribe it. Many states that have allowed independent prescribing include training recommendations in the legislation to address this concern, although a survey of medical and pharmacy students found no difference in PrEP knowledge between the disciplines. Studies that compared pharmacist-led PrEP clinics to physician-led clinics found similar patient retention rates in both settings.
Legislative Best Practices
Simply authorizing pharmacists to prescribe PrEP independently will not ensure that pharmacies choose to offer this service. There are a few legislative best practices that can make it more feasible for pharmacists to offer PrEP prescribing as a service.
- Ensure that legislation allows pharmacists to order, interpret, and bill insurance for laboratory tests and receive reimbursement for PrEP services.
- Make legislation flexible enough to account for new forms of PrEP that may be approved in the future.
- Specify that pharmacists can administer, not just prescribe, long-acting injectable PrEP.
- Ensure that the pharmacist can prescribe a large enough supply of PrEP to cover a patient through the referral process, if required. For example, in 2024, California updated their PrEP prescribing legislation to extend the prescription length from a 60-day supply to a 90-day supply.
Conclusion
Increasing PrEP use has decreased the HIV diagnosis rate in the United States. Although PrEP coverage has increased since 2019, and more states are allowing pharmacists to independently prescribe PrEP, there is room to improve. For policymakers considering expanding pharmacists’ scope of practice to include prescribing PrEP, legislative models already exist. Evidence shows that consumers are interested in being able to get a PrEP prescription from a pharmacist and that pharmacist prescribing may reach people who otherwise might not explore PrEP as an option. Although HIV is no longer the death sentence that it was when it was first identified, preventing new HIV infections remains important. Allowing pharmacists to prescribe PrEP is one policy strategy that can help end the HIV epidemic.
Our Integrated Harm Reduction Team
Our program focuses on harm-reduction approaches that recognize that harmful behaviors may continue to happen even as policies are enacted to help mitigate—if not eliminate—those harms. We connect the dots between historically siloed issues such as: tobacco, cannabis, sexual health, and illicit drug use.
